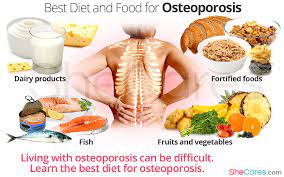
Eating a healthy diet rich in essential nutrients such as calcium, vitamin D, and protein can help reduce the risk of osteoporosis. In addition, limiting caffeine and alcohol intake may be beneficial for bone health, especially among older adults.
Worldwide, 1 in 3 females and 1 in 5 males over the age of 50 will be affected by a broken bone due to osteoporosis, and osteoporosis or low bone mass affects 54%Trusted Source of Americans.
A person’s diet can affect bone health, so people must consider nutrition to maintain their bone mass.
This article discusses how nutrients affect the bones and which foods are best to eat and avoid.
Bone does not remain static throughout life — it is constantly breaking down and rebuilding as part of normal bone metabolism.
Two main types of cellsTrusted Source, osteoblasts and osteoclasts, participate in this process. Osteoblasts form new bone, while osteoclasts break down old bone in a process called resorption.
However, if bone metabolism becomes unbalanced, bones can become less dense, weaker, and brittle. As a result, a doctor may diagnose low bone mass or osteoporosis.
Several factorsTrusted Source can cause bone loss, including aging, menopause, and certain medications.
Moreover, consuming key nutrients for bone health can help to reduce the risk of osteoporosis and keep bones healthy.
Individuals should ensure to include the following nutrients and foods in their diet to keep bones healthy:
Calcium
The National Institute of Arthritis and Musculoskeletal and Skin Diseases advises that low calcium intake throughout life has an association with low bone mass and high fracture rates.
From 51 years, females require 1,200 milligrams (mg) of calcium daily, and males need 1,000 mg.
People can ensure they consume calcium by including dairy or soy products, fish with bones, and leafy green vegetables in their diets.
The following shows the calcium content of some common foods:
- fortified oatmeal, packet: 350 mg calcium
- sardines, canned in oil, with edible bones, 3 ounces (oz): 324 mg calcium
- cheddar cheese, 1.5 oz, shredded: 306 mg calcium
- milk, nonfat, 1 cup: 302 mg calcium
- tofu, firm, with calcium, 0.5 cup: 204 mg calcium
- orange juice, fortified with calcium, 6 oz: 200–260 mg calcium
- baked beans, 1 cup: 142 mg calcium
Vitamin D
The body needs vitamin D to absorb calcium, and a deficiency of vitamin D could cause the weakening of the bones and skeleton.
Experts recommend that individuals up to 70 years have a daily intake of 600 IU (International Units) of vitamin D.
People over age 70 should increase their uptake to 800 IU daily, which they can also obtain from supplements.
People can get vitamin D from sunlight and food. The following foodsTrusted Source contain vitamin D:
- egg yolks
- oily fish such as salmon, trout, mackerel, and tuna
- beef liver
- cheese
- mushrooms that producers have treated with UV light
- milk, margarine, orange juice, and cereals that manufacturers have fortified with vitamin D
Protein
Research suggests that protein can be both beneficial and detrimental to bone health, as different studies have produced different results on the effects of protein on bone health.
However, according to the Framingham OsteoporosisTrusted Source study, there is a link between low protein intake and greater bone loss and hip fractures in older adults.
The study concluded that the combination of sufficient protein and calcium intake appears to benefit bone mineral density (BMD).
Therefore, eating a diet with sufficient protein and calcium seems wise. Protein-rich foods include:
- meat
- fish
- eggs
- dairy products
- beans, lentils, and legumes
- soy products
- seitan
- nuts and seeds
Micronutrients and antioxidants in fruits and vegetables
The Framingham Osteoporosis Study identified that people with a higher fruit and vegetable intake had better BMD and less bone loss.
The nutrients in fruits and vegetables that the study indicated are beneficial to bone health includeTrusted Source:
A 2017 cross-sectional studyTrusted Source of Chinese people aged 40–75 years found that a higher fruit and vegetable intake correlates with higher BMD and lowers the risk of osteoporosis.
Additionally, a 2019 meta-analysisTrusted Source found moderate-quality evidence that increasing a person’s fruit and vegetable intake by at least one serving per day decreases the risk of fractures.
Foods to limit or avoid
In addition to eating a healthy diet to support bone health, people should be aware of some detrimental foods and drinks.
Salt
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, overconsumption of salt can cause the kidneys to excrete calcium.
Therefore, people who have a low calcium intake should avoid adding salt to food or eating too many processed foods that can contain excess salt.
Foods containing oxalates and phytates
The Bone Health and Osteoporosis Foundation advises that some substances in food can interfere with the body’s ability to absorb calcium.
These include phytates in beans, wheat bran, and legumes and oxalates in spinach and beets. Soaking and cooking these foods can help to reduce these compounds.
Alcohol
Experts advise that alcohol negatively affects bone health for several reasons.
Firstly, drinking excessive alcohol can interfere with the body’s absorption of calcium and vitamin D.
In addition, chronic heavy drinking can disrupt hormones, such as elevating cortisol levels, which can break down more bone. Males may produce less testosterone, a hormone that has links to bone formation, while females may notice irregular menstrual cycles. Irregular menstrual cycles can reduce the amount of estrogen in the body, which increases the risk of osteoporosis.
Moreover, people under the influence of alcohol are more at risk of falls and bone fractures.
Caffeine
A 2021 study found that 800 mg of caffeine consumed in 6 hours increased the clearance of calcium by the kidneys by 77%Trusted Source.
An older studyTrusted Source suggests that as coffee may increase the amount of calcium the body excretes in urine, people should not drink more than three cups per day, especially if they are older.
Additionally, the Bone Health and Osteoporosis Foundation advises that caffeine in soft drinks such as colas can have the same adverse effects.
Learn 11 ways to increase bone density naturally.
Summary
To protect bones throughout life, people should eat a healthy diet containing essential nutrients and engage in physical activity.
Calcium, vitamin D, and protein are vital protective nutrients and vitamins, minerals, and antioxidants in fruit and vegetables.
Older adults may wish to limit coffee to three cups per day and avoid excessive alcohol.
Avoiding excessive alcohol and salt may be beneficial for everyone for overall health and well-being, especially those who have limited calcium intake.