- Holiday feasting can leave you feeling bloated and uncomfortable.
- Experts share ways to ease your stomach discomfort this holiday season.
- Knowing your triggers, swapping foods, and limiting alcohol can all help make holiday meals more pleasant.
A full and heavy belly can mean great things were just consumed, but it can also mean uncomfortable things are about to happen.
For many Americans, that feeling is just par for the course during holiday celebrations.
According to research from the Calorie Control Council, a typical Thanksgiving dinner is packed with over 3,000 calories. That’s almost double the recommended calorie intake for adult women based on the 2020-2025 Dietary Guidelines for AmericansTrusted Source.
And stomachs can only hold so much food before they hit their capacity.
For instance, on average, an adult’s stomach is similar in size to a clenched fistTrusted Source. It can hold about 2.5 ounces if it’s emptyTrusted Source and expand to hold around 1 quart.
As you fill your stomach up to its capacity, doing so can cause discomfort, including indigestion and even nausea.
To help banish that overfed, lethargic, bloated feeling, nutrition experts say the following 5 tips can help reduce intestinal discomfort during the holiday season.
1. Recognize your triggers
As a guest of a party, you might find yourself at the mercy of what the host is serving, which can mean you might not know exactly what ingredients they are using to prepare their food.
However, knowing ahead of time what ingredients trigger discomfort can help eliminate bloat.
“Whether it’s dairy, gluten, or some other food, being aware of food intolerances and other triggers is important so you can avoid or limit them in order to prevent digestive issues like bloating,” Michael Hartman, PhD, nutrition expert, told Healthline.
He suggested asking the host before the party what they intend on serving and what ingredients are in the food.
“The last thing they want is for you to feel unwell,” said Hartman.
To identify foods that trigger bloat, Erin Palinski-Wade, registered dietitian and author of Belly Fat Diet For Dummies, recommended keeping a daily food record and looking for patterns.
“It is best to track the food you eat, the portions, the timing, emotions at the time (happy, stressed, etc.) as well as any symptoms you feel,” she told Healthline. “This can allow you to look for patterns to identify foods that may cause bloat as well as help you to see if other factors such as stress may be aggravating your symptoms.”
2. Don’t save calories for the party
Eating consistently throughout the day can help keep you from over-eating at the party.
“Waiting too long in-between meals until you are ravenous can often lead to eating too fast and too much, which can trigger an increase in bloating,” said Palinski-Wade.
Instead of “saving” all your calories for a big meal, she said to eat consistent meals and snacks to support digestion throughout the day.
“Watch out for foods that may trigger bloat, such as large amounts of cruciferous vegetables at one sitting, eating more fiber than you generally would without building up, or eating meals with large amounts of fats, sodium, and added sugar,” she said.
3. Make food swaps
Whether you’re the host or know what the host will be serving at the party, you can provide alternative options to choose from.
“If you’re trying to build a healthy relationship with food, there are simple healthy holiday food swaps you can make,” said Hartman.
For instance, if dairy-filled cheese balls and crackers are a typical appetizer at your holiday dinner table, he said to try mixing it up this year with hummus, pita, and fresh veggies.
Instead of buttery mashed potatoes, consider switching to a sweet potato alternative.
“And, rather than going for a rice dish that’s high in starch, reach for legumes which are rich in potassium, a mineral that helps flush out excess bloat-causing sodium,” Hartman said.
Palinski-Wade suggested using milk in replacement of heavy cream to cut the fat in recipes and reduce large amounts of salt by using flavorful spices like cinnamon and nutmeg.
If swapping feels overwhelming or like too much work, she said to stick to eating in moderation. Her favorite strategy for doing this at holiday meals is to review all food offerings first before adding them to her plate.
“Then build a balanced plate filling 1/3 with produce, 1/3 with lean protein, and the remaining 1/3 with any favorite side dishes,” she said. “This allows you to enjoy all the offerings without overdoing it, which can help reduce bloat.”
3. Make food swaps
Whether you’re the host or know what the host will be serving at the party, you can provide alternative options to choose from.
“If you’re trying to build a healthy relationship with food, there are simple healthy holiday food swaps you can make,” said Hartman.
For instance, if dairy-filled cheese balls and crackers are a typical appetizer at your holiday dinner table, he said to try mixing it up this year with hummus, pita, and fresh veggies.
Instead of buttery mashed potatoes, consider switching to a sweet potato alternative.
“And, rather than going for a rice dish that’s high in starch, reach for legumes which are rich in potassium, a mineral that helps flush out excess bloat-causing sodium,” Hartman said.
Palinski-Wade suggested using milk in replacement of heavy cream to cut the fat in recipes and reduce large amounts of salt by using flavorful spices like cinnamon and nutmeg.
If swapping feels overwhelming or like too much work, she said to stick to eating in moderation. Her favorite strategy for doing this at holiday meals is to review all food offerings first before adding them to her plate.
“Then build a balanced plate filling 1/3 with produce, 1/3 with lean protein, and the remaining 1/3 with any favorite side dishes,” she said. “This allows you to enjoy all the offerings without overdoing it, which can help reduce bloat.”
4. Add leafy greens to your plate
Vegetables like spinach, kale, bok choy, asparagus, and chard have a high-water content and are also low in calories and packed with vitamins, minerals, and fiber. “[They] work well to reduce bloating,” said Hartman.
While eating vegetables regularly is a great way to add fiber to the diet, Palinski-Wade cautioned that increasing fiber gradually is the best way to promote healthy bowel movements and reduce bloat.
“If you increase your vegetable intake quickly without adjusting to an added fiber intake, this may result in more bloat,” she said. “Also, if you do not increase your water intake as you increase fiber, this can lead to bloat and constipation as well.”
She recommended adding an extra half cup of leafy greens every 3 days to slowly increase your intake to improve digestion without the bloat.
“Cruciferous vegetables like broccoli can cause more gas as well, so these are often best to enjoy cooked versus raw to lessen the impact on bloat,” said Palinski-Wade.
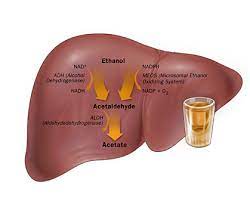
5. Limit alcoholic drinks
While alcoholic drinks are often part of celebrating the holidays, drinking alcohol after eating heavy meals can make a swollen stomach worse.
“Alcohol is an inflammatory substance that can slow digestion and increase water retention, making you feel lethargic. It can also lead to swelling in the body, which can result in gas, discomfort, and bloating,” said Hartman.
To prevent dehydration and up your water intake, Palinski-Wade said to leave visual reminders like setting your water bottle out where you can see it during the day. She also suggested setting an alarm on your phone to encourage you to sip on water or use an app to track your intake.
“Spacing water out helps to prevent bloat, but don’t try to chug water all at once since that may increase bloat as well,” she said.
To moderate alcohol intake, Palinski-Wade said it’s best to keep to drinking one glass of an alcoholic beverage for women and two glasses for men per day. Plus, for every glass of alcohol you consume, drink at least one glass of water.
“During holiday celebrations, try incorporating fun mocktails made with sparkling water and 100% juice as a delicious way to enjoy the celebration without the added bloat the next day,” she said.
Her favorite go-to concoction is 1 cup of seltzer water with ¼ cup tart cherry juice and a slice of lime “for an antioxidant-rich drink that looks just like a fancy glass of wine.”
Hartman suggested ditching the mulled wine and spiked eggnog and opting for a nonalcoholic cider or punch instead.