World No Tobacco Day is observed on May 31 every year since 1987. This year, the World Health Organization’s (WHO) theme for the Day is “Tobacco: Threat to our environment.” This drive aims to create awareness among the public on the detrimental impact of tobacco cultivation, production, distribution, and waste on the environment, besides human health.
According to WHO, about 3.5 million hectares of land are cleared for growing tobacco each year. It causes deforestation mainly in the developing nations. Tobacco cultivation results in soil degradation, making it infertile to support the growth of other crops or vegetation. Tobacco contributes 84 megatons of the greenhouse gas carbon dioxide to the atmosphere every year; around twenty-two billion litres of water is consumed in the production of cigarettes every year.
The situation is no different in India, where tobacco is one of the important cash crops. Today, India is the second-largest crop producer in the world after China. According to the Central Tobacco Research Centre of the Indian Council of Agricultural Research (ICAR), around 760 million kg of Tobacco is grown in India on about 40 lakh hectares of land. The sector provides jobs to millions of people and contributes as much as Rs.22,737 crore as excise duty and Rs.5,969 crore in foreign exchange to the national treasury.
But a massive cost of tobacco cultivation is paid for by the country’s environment and people’s health. A report by the Ministry of health and family welfare says that “The total economic costs attributable to tobacco use from all diseases in India in the year 2011 for persons aged 35-69 amounted to Rs. 1,04,500 crores”.
It is estimated that about 29% of the adult Indian population consumes Tobacco. Most commonly, it is consumed as Smokeless Tobacco Products like khaini, gutkha, and zarda. Smoking forms of tobacco are used as bidi, cigarette, hookah, etc. The smokeless forms pose high risks of oral and oesophageal cancer. Their consumption by pregnant women can also lead to stillbirth and low birth weight in infants. People addicted to smoking are, on the other hand, at very high risk of lung, oral cavity, pharynx, nasal cavity, larynx, esophagus, stomach, pancreas, liver, kidney, ureter, urinary bladder, uterine cervix, and bone marrow cancers.
Tobacco kills more people than tuberculosis, HIV/AIDS, and malaria combined worldwide. It has also been reported that tobacco consumption in both smoking and chewing forms is significantly associated with severe COVID-19 symptoms. Tobacco users’ pre-existing health conditions, such as respiratory and cardiovascular disease, were observed to exacerbate disease symptoms, making treatment of COVID-19 patients more difficult owing to their fast clinical deterioration.
The environmental impacts of tobacco cultivation also add to India’s enormous economic burden. Tobacco is a very nutrient-hungry crop, and it depletes soil nutrients more rapidly. Tobacco cultivation requires the application of pesticides and fertilizers in large amounts, which degrade overall soil health. Tobacco cultivation results in soil erosion because it is typically grown as a monocrop (the practice of cultivating a single crop on the same farmland year after year), exposing the topsoil to wind and water.
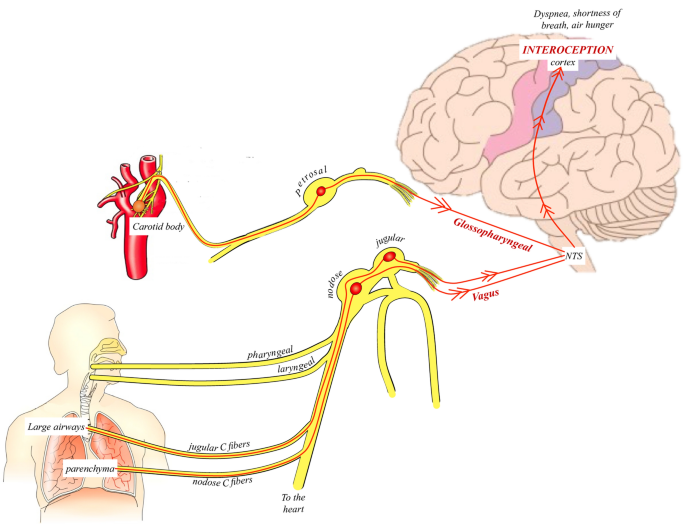
Besides, health risks are associated even with tobacco cultivation apart from consumption. Tobacco farmers are prone to suffer from a work-related ailment known as “Green Tobacco Sickness” (GTS), which is caused mainly by nicotine absorption via the skin. Nicotine is an addictive chemical found in tobacco. The studies carried out by the National Institute of Occupational Health (NIOH) on CTRI farms in Andhra Pradesh reveal discoloration of workers’ skin coming into contact with tobacco leaves. Headache, nausea/vomiting, dizziness, lack of appetite, exhaustion, and weakness are all signs of GTS, which can be caused even by tobacco storage in houses. Severe nicotine poisoning can adversely affect reproductive health and lead to breathlessness, blood pressure fluctuations, heart attack, and cancer.
To cope with the tobacco epidemic, the Government of India enacted an extensive tobacco control law: The Cigarettes and Other Tobacco Products Act 2003 (COTPA 2003), in 2004. This Act includes the prohibition of smoking in public places, advertisement of cigarettes and other tobacco products, sale of cigarettes or other tobacco products to anyone below the age of 18 years, and prohibition of selling areas like schools, colleges, etc.
To make India addiction-free, the Government has launched programmes like National Tobacco Control Programme and Nasha Mukt Bharat Abhiyaan. Department of Agriculture, Cooperation & Farmers Welfare is also implementing a crop diversification programme. Farmers are encouraged to replace tobacco crops with less water-consuming alternatives to conserve water and soil. Under irrigated conditions, sugarcane, onion, maize, etc., and under rain-fed conditions, groundnut and soybean could be potential alternatives to tobacco farming.
The WHO’s this year’s campaign on “Tobacco: Threat to our Environment” urges governments and policymakers to strengthen legislation and implementation of existing schemes that hold tobacco companies accountable for the environmental and economic costs of waste tobacco products.